|
I felt like a movie star years ago, walking into the Sean Parker Voice Institute in New York City. The halls were lined with signed photographs from famous actors and singers. Not being able to carry a tune made me feel out of place, but, hey, I was there to find out why I was often hoarse.
While I was sitting on the exam table, talking to the doctor, I cleared my throat. “Don’t do that!” she said. “Clearing your throat is harsh on your vocal cords and can cause inflammation. Instead take a sip of water. And, if you don’t have water available, try to suppress the urge.” I’ve done pretty well over time and I must say I clear my throat very infrequently now. Recently, reading an Instagram post by Dr. Inna Husain, an ENT, I see she also says throat clearing is a no-no. In addition to taking a sip of water she suggests if we don’t have water available to do a hard swallow. She explains that clearing our throat can traumatize our vocal cords and create a hypersensitivity and mucus. Dr. Husain suggests using .9 % saline to moisten our vocal cords. And, of course, many of us are already nebulizing for our bronchiectasis and I imagine nebbing salty saline could actually irritate our cords!!! 😱😱😱 Perhaps we could ask our medical team if it makes sense when we find ourselves clearing our throat a lot, to moisten our cords by nebulizing with .9 isotonic solution. Also, I suggest becoming more aware of when we clear our throat and to try to suppress the urge. Come up with a few ways of dealing with it, such as sucking a non-mentholated candy, taking a few puffs on Aerobika or drinking water. #throatclearing #chronicthroatclearing #mucus #phlegm #coughing #bronchiectasis #nebulizing
0 Comments
Some with BE take showering precautions to limit exposure to steam that can harbor lung pathogens. This concern can make traveling tricky. So, let’s brainstorm about our bathing and showering options!! One solution is to find accommodations that have a bathtub. Another is to see if the accommodations have showers with a handheld fixture that allows one to target the water and minimize steam exposure. This is my go-to method in my NYC apartment, and it works great! In addition, think about the following: *Let your tap, toilet and shower run for several minutes before using water (don’t be in the room while clearing out the pipes) *Run a bathroom fan while bathing *Take short showers *Substitute sponge baths for showers *Wear a mask *Remove the showerhead as it is often the source of bacteria I recently heard from someone who brings his own showerhead! Now I call that planning a “head”:)!! Whatever our challenges, let’s be sure to not make them obstacles to enjoying ourselves. #showerprecautions #drfalkinham #maclungdisease #ntmlungdisease #bronchiectasis Some of us with bronchiectasis choose to take drinking water precautions to prevent bacterial infections. We drink water that is sterile. Options are:
*Water from a Lifestraw pitcher or water bottle with filters (NOT a Brita filtering device). *Water from a UV water bottle or treated with a Steripen *Bottled spring water *Boiled water When traveling, some of these options might not be available or practical, but generally speaking, we can find one that works for us. I used the Steripen regularly during my trip in October to Italy and also when necessary bought bottled water. I chose not to bring my Larq UV water bottle on my trip because while sightseeing I don’t like carrying anything or wearing a backpack. But, many find it and the CrazyCap helpful. Now let’s talk about how the water we drink can cause an infection in our lungs and possibly more bronchiectasis. The answer is two-fold: by inefficient swallowing and gastric reflux. All of us micro-aspirate liquid into our lungs throughout the day. This might be from liquid “going down the wrong pipe” as can happen with swallowing issues and coughing. Gastroesophageal reflux is another way bacteria can enter the lungs. Both acid and non-acid gastric refluxate can come up from the stomach and enter the lungs. One way to help prevent reflux while traveling is to take precautions including: *Raising the head of your bed *After eating, waiting a couple of hours before lying down, doing airway clearance or exercising *Squatting down instead of bending at the waist whenever possible *Not eating trigger foods Not everyone with bronchiectasis will get a lung infection. However, there is about a 25-30% chance one will and the precautions I have laid out can reduce that probability. In Italy, I found that most restaurants were filtering their own water to cut down on plastic use. I preferred not to drink their water as I assumed it probably was not sterile. Surprisingly, quite a number of the restaurants no longer served bottled water. So, wherever you journey to, be prepared for eco-friendly restaurants by bringing your own water. #lunghealth #lunginfectionprevention #falkinham #Bronchiectasis #NTMDisease #MACDisease #Falkinham #macdisease #mucusinbackofthroat #GERD #SwallowingDifficulties #sterilewater #lifestraw Planning for a trip? Here’s how to pack smartly for your self-care needs, especially those related to airway clearance.
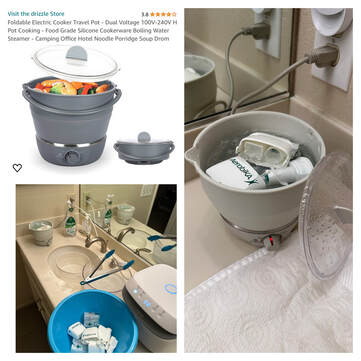
Know your limits: Consider how many bags you can handle comfortably. If you’re flying solo, packing light is key! Pack a carry-on specifically for your healthcare needs. Most airlines allow a medical bag with a doctor’s note. To vest or not to vest? Some people rely heavily on their airway clearance vest and will need to take it along on all trips and others have the option of traveling without it. Talk to your medical team about travel options without the vest. Vest companies often stipulate that vests be carried onboard and not checked. My Italy Packing List : 3 sets of nebulizer cups and Aerobikas 60+ vials of hypertonic saline (1 month) Pari Trek S Travel-sized nebulizer Innospire Go Battery-operated nebulizer (unreliable) Massage gun* Exercise stretch band Rescue antibiotic A nebulizer compressor tubing replacement *I chose not to bring my vest to Italy Sterilization on the go: Medela microwave steam bags Pack a small bottle of isopropyl alcohol for sanitizing Use resealable plastic bags for soaking and sterilizing equipment (Marjorie Cullinan, Yale Respiratory Therapist) Bonus tip: Consider a dual-voltage travel steamer (like the foldable “Drizzle Pot”) for easy sterilization on the go! Remember: This is just a guide! Adapt it to your specific needs and discuss your travel plans with your medical team. Best tip of all is to BOARD EARLY!! The first time I did it, I felt a little foolish, but it made all the difference. You’re not blocking the aisle as you try to get all of your stuff organized. Happy travels! Please share this blog site in your support groups, especially with people who are not on social media. I thank you in advance! #bronchiectasis #travel #bronchiectasiswarrior Struggling with lung issues? Choosing the right nebulizer setup can make a big difference! Several years ago, I upgraded to the Ombra system from Monaghan and Trudell International.
This more powerful system is what National Jewish Health (NJH), a top US lung hospital, recommends to their patients. While I haven't received care there myself, I trust their expertise. As a BE consultant, I often hear what clients treated at NJH are instructed to do. In all cases, they've been advised to use an Aerobika with an Aeroelipse XL cup and an Ombra compressor. It's important to note that patients are also advised to change the tubing regularly (every 2 months to 2 weeks depending on source) and the filter every 6 months to maintain optimal performance. While there are other good nebulizer options from Pari and Philips, each system delivers medication differently. Substituting one cup for another can affect how much medication you receive. Talk to your doctor about the best nebulizer setup for your specific needs. #bronchiectasis #lunghealth #nebulizer #nebulising #nebulizing #nebulise #aerobika #aeroeclipse #paritreks A LETTER OF APPRECIATION TO MY DRIZZLE POT
Dearest Drizzle, I apologize for calling you "glitchy" back in October while I was in Italy. It seems I malfunctioned, not you! I thought I had read the instructions carefully, but I missed the crucial step about needing to flip you upside down and change the voltage when abroad. While using you in our California rental, you've been working wonderfully. Thank you for being such a reliable companion! Please forgive me, Linda #drizzlepot #airwayclearance #bronchiectasis #travelingwithbronchiectasis This week we'll dive into travel essentials and how to pack them!
But first, a tip: budget $200 for self-care equipment. Why? Because:
Equipment Sourcing Guide– *Steripen - Amazon (lithium batteries need to be in carryon) *Medela steam bags - Amazon *Dr Brown steam bags - Amazon *Drizzle foldable electric travel pot - Amazon *Aerobika with manometer - Allied Medical Express *Aerobika (no manometer) - SaveRite *Pari Trek S portable nebulizer system - SaveRite *Inflatable wedge *My book “The BE CLEAR Method to Living with Bronchiectasis.” For motivational reading!!! *Battery operated nebulizer I do not have a suggestion for one over another. You will need to plan on using a cold method of sterilizing as most of them cannot withstand high heat. What you bring on your trip will depend on whether you are flying, taking a train, bus or car. Also, how much luggage you are allowed to take without a surcharge or even have space for. Additionally, how many luggage pieces can you comfortably handle? If you are traveling outside of the US, you will need a plug adaptor and perhaps a voltage converter. It is always best to check with the electrical device manufacturer to know whether their equipment will work on your travels. The Ombra nebulizing system is meant only for the US and Canada. The Pari Trek S portable compressor comes with Sprint nebulizing cups that can withstand high heat. It is not as powerful as the Ombra, but will get the job done. Test before you go! Don't wait until vacation to discover your new equipment isn’t reliable. Try everything beforehand for a stress-free trip. Remember, investing in your health makes a world of difference! #bronchiectasis #traveltips #selfcare #chronicillness #airwayclearance In a previous post, we discussed the importance of pre-travel exercises for everyone. But for those managing bronchiectasis, preparing our body with stretches and strength training is extra important!
Traveling often involves lifting luggage, long journeys, and unfamiliar environments, so being in good shape can make a big difference. But that’s not all! Effective communication plays a vital role too. Talking openly with your travel companions about your airway clearance needs and rest requirements can be a game-changer. Let them know you might need to schedule specific times for these activities or even stay back at the hotel sometimes. Most importantly, don’t forget to have a conversation with yourself!! As much as we try to keep all of our procedures in place, including exercise, airway clearance, healthy eating, and perhaps time for meditation and other non-sleep relaxation practices, sometimes there isn’t the time nor the energy for them on vacation. It can be disturbing when this happens. But the reality is it’s probably going to happen repeatedly on vacation. What I try to do is monitor my mood so I don’t get grouchy. I stay calm about it with a five-minute relaxation exercise in the morning or even the night before a big travel day. And I prioritize what I think is the most important of my self-care practices. On a month-long trip to Italy within the first few days I got a cold. So it was easy to prioritize air clearance over exercise because I always take my exercise down a notch when I don’t feel well. I make sure to walk and move, but I’m less likely to do structured exercise. Also, I did something I’ve never done before and took my rescue antibiotic on day 5 of producing more sputum than my usual. Again, not something I wanted to do and I would not have done it at home. I would’ve had a sputum culture before taking an antibiotic. By taking the time to have these conversations beforehand, you’ll be laying the groundwork for a smoother, more enjoyable, and ultimately, more memorable trip for everyone involved. Letsbecleartoday.com #chronicillnesstravel #bronchiectasiswarrior #bronchiectasisawareness #lifebeyondbronchiectasis #bronchiectasis #invisibleillness #mentalhealthmatters This week, we’re diving into the world of traveling with bronchiectasis. While packing tips are coming (trust me, I’ve got you covered!) let’s talk about an even more crucial aspect: strengthening and stretching your body. Imagine navigating cobblestone streets with a nebulizer backpack, suitcase, and chest vest. Sounds tiring, right? The last thing you want while traveling is to throw out your back. So, before your adventure begins, consider dedicating some time to building strength and improving flexibility. This isn’t just about your back, but about creating overall strength from head to toe. Why is this important? A strong body will help you: *Effortlessly lift luggage into overhead bins, taxi trunks, and hotel room suitcase stands. *Maneuver wheeled suitcases with ease. *Maintain good balance and prevent falls. Beyond packing tips, “packing on” some muscle and strength can make a real difference. My book, “The BE CLEAR METHOD to Living with Bronchiectasis,” features 10 straightforward exercises that, done consistently, can significantly improve any travel experience. Remember, exercise does more than help with travel; it’s crucial for overall health and well-being. So, while you’re planning your trip, consider incorporating some strengthening and stretching into your routine. Ready to learn more? Check out my book for those 10 essential exercises (GERD-friendly), or get in touch for personalized guidance! https://amzn.to/3C18rl1 www.letsbecleartoday.com #exercise #strongbody #personaltrainer #stretch #strength #Bronchiectasis #COPD #Asthma #CysticFibrosis #LongCovid #Mucus ⭐️⭐️BE-Practical Series⭐️⭐️
Oral microbiota is a hot research topic and within the next five years we will hopefully have a better understanding of the role these bacteria play in the lung microbiome. Although it is hard to believe, we have over 700 different types of bacteria in our mouths! Some are good, some not so good and some we aren’t sure of. For those of us who have dealt with NTM infections like MAC, the good news is NTM are generally not found in the oral cavity. However, when we cough and secretions enter our mouth, they could end up on our toothbrush. A dab of dish soap and a scrubbing will help clean your toothbrush, and if you have a baby bottle sterilizer, you might see if your toothbrush can withstand the heat. My client put his toothbrush in a microwave bag for three minutes and it bent, so I would avoid this method or try it for a shorter time. I recently treated myself to this mini UV device I found on Amazon. I pop my toothbrush into it after each use and also take it on trips. It isn’t a “must-have” device, but it is reasonably priced and easy to use. In addition, its a good idea to maintain a healthy mouth with good oral hygiene and regular dentist visits. Don’t forget to get your complimentary toothbrush from the hygienist! You might want to consider using a new one every month. #oralhygiene #toothdecay #bronchiectasis #dentistvisits #uvsterilizers #ntm #ntmlungdisease #maclungdisease #cysticfibrosis #pseudomonas #haemophilus |
AuthorLinda Cooper Esposito, MPH is a health educator with bronchiectasis. She developed the BE CLEAR Method to Living with Bronchiectasis and writes with compassion and humor about this chronic lung disease. Archives
March 2024
Categories |












 RSS Feed
RSS Feed