|
Bronchiectasis, or BE, cannot be cured. The disease causes the lungs to scar and can happen to anyone after a respiratory illness or with conditions such as Chronic Obstructive Pulmonary Disease (COPD) and Cystic Fibrosis. With the pandemic, we will likely see a sharp increase in the number of individuals with bronchiectasis. Until recently, bronchiectasis was considered a rare disease with less than 200,000 cases in the United States. However, with the increased use of High-Resolution Computerized Technology (HRCT) scans as well as a heightened awareness in the medical community, bronchiectasis is being diagnosed more than ever. Researchers now suggest that a significant percentage of the 20 million COPD sufferers in our country also have undiagnosed BE. Although BE is a permanent condition, it can be effectively managed and its spread mitigated or even prevented. Based upon my personal experience with bronchiectasis and professional experience as a health and fitness educator, I have developed the BE CLEAR Method. Together with traditional medical treatments of the disease, the BE CLEAR Method empowers individuals living with BE to be actively involved in their own care. The overarching goal of the method is to sustain healthy lungs while building a stronger body and mind to meet the daily and life-long challenges of our disease. Through dedicated practice, the BE CLEAR Method becomes not just a road map but a travel companion for those living with bronchiectasis. The two key elements of the BE CLEAR Method are exercise and airway clearance both of which help remove harmful mucus from the lungs. The method also employs a broader approach including effective breathing and meditation practices to deal with the anxiety and depression that is common among people with chronic health conditions. In addition, better relaxation and sleeping habits are discussed as well as the importance of a nutritious diet to maintain a sound body and mind. Mystery surrounds bronchiectasis. Many of the afflicted do not know how they got it. Those I have talked to in support groups on-line and in-person want clarity. Most of all, they want to feel better. As someone who shares in their struggle, as someone who lives with BE every day, it breaks my heart to hear their stories. That’s why I wrote The BE CLEAR Method to Living with Bronchiectasis. I want to share with others the practices I have used for years to stay full of energy and positive-minded. I encourage people with BE to stay on task and do the daily work. At the same time, I point out that we are all at different points along the health continuum and we need to move forward from our unique place. In BE CLEAR, I weave current evidence-based research into my own story with humorous anecdotes that they will recognize and appreciate. Ultimately, my goal in writing this book is to show people living with BE that they have more control over their disease than they think. With the regular application of the BE CLEAR Method, they can lead a full and joyful life. The “BE CLEAR Method to Living with Bronchiectasis” is available on Amazon. https://amzn.to/3maqeAB #bronchiectasis #airwayclearance #lungdisease #maclungdisease
0 Comments
About 25% of people with bronchiectasis will at some point develop a Pseudomonas aeruginosa infection. The older we are, the more widespread our bronchiectasis and the poorer our lung function, the more likely we are to get this type of infection.
During the recent European Lung Foundation Bronchiectasis Patient Conference 2022, Dr Josje Altenburg from Amsterdam discussed whether this infection should be treated. She asked—”Is the Pseudomonas a threat or a pet?” Have a listen-- https://www.youtube.com/watch?v=_bNlHxTIY14 It is important to understand the issues Dr Altenburg presents in the event we repeatedly grow Pseudomonas in our sputum cultures. I found her talk about new therapies to eradicate Pseudomonas fascinating, especially the possible use of monoclonal antibodies and bacteriophages. Regular sputum cultures are critical for good health as sometimes there are no indications that Pseudomonas is causing an infection. However, particularly for those of us who have had these infections in the past, we might notice health changes such as fatigue, coughing and more sputum production. Additionally, for some, our sputum might turn greenish and have a strong odor. A key to living with bronchiectasis is understanding the nature and management of the disease and the pros and cons of treatments. Being acquainted with the issues puts us in the driver’s seat. In the future, if we are presented with challenges, we can further educate ourselves and along with our medical team, make well-informed decisions. #pseudomonas #lungdisease #bronchiectasis #airwayclearance #sputum #mucus #phelgm #lunginfection #lunginflammation Aches and pains? Posture not the best? Coughing and short of breath? The answer might just be...a fanny pack!!
Carrying a bag, even a cross-body one, can throw off your gait, body mechanics and the ability of your rib cage to expand. It’s important to be evenly weighted, unencumbered and allow your arms to swing freely. Walking this way is how the body reorganizes and naturally releases tight muscles. So, think twice before carrying a bag of any type in one hand or on one shoulder for a length of time. And, yes, a fanny pack might be part of the solution. Every now and then, switch it to the other hip or better yet, center it! #Lung #LungHealth #Breathing #Breathe #Bronchiectasis #COPD #Asthma #Emphysema #ChronicBronchitis #posture #chroniccough In 2017, after I was diagnosed with bronchiectasis and a MAC lung infection, I spent months walking around in my Upper Westside neighborhood in a daze. At the time, I was seeing a pulmonologist who hadn’t explained anything to me in detail. To make matters worse, it seemed like the more I researched these two rare conditions online, the more questions I had.
Fortunately, my emotional brain fog did not prevent me from seeking answers from other professionals. The first breakthrough I had was meeting with Marion Mackles, a cardiopulmonary expert at the Pulmonary Rehabilitation and Wellness Center. She patiently answered my questions and taught me airway clearance techniques. I liked the friendly vibe at the center and over time I followed up by watching many of the Pulmonary Wellness seminars that were offered at no charge (and still are!). One of my favorites was Dr. Noah Greenspan, owner of the center, interviewing Donna Wilson, a Registered Respiratory Therapist, nurse and clinical exercise specialist. After listening, I knew I needed to see her for a consultation. At the time Ms. Wilson was working in the Integrative Health department at Memorial Sloan Kettering. We met and went over my CT scan report and health issues. She answered questions and together we did exercises that target the breathing muscles, including strengthening the diaphragm, which plays a large role in respiration. I have continued to do her exercises over the years and thought she had retired. So, I was so pleased to see a Pulmonary Wellness social media post at the beginning of this year saying that she would again be a guest speaker. Now, the recording is available! https://vimeo.com/710460803 I promise you, it will make you reconsider how you breathe and the critical role of exercise! As always, consult your medical team before beginning, modifying or stopping exercise. Oh, did I mention you will never see another woman in her 70’s with such incredible arm muscles? #pulmonarywellness #bronchiectasis #copd #asthma #breathing #oxygen #exercise #healthylungs Steroids and Inhaled Corticosteroids (ICSs) can cause osteoporosis and increase the risk of infections. Some of us with bronchiectasis take steroids and ICSs because of other medical conditions. In addition to BE we might have comorbidities such as rheumatoid arthritis, asthma, COPD and inflammatory bowel disease (IBS).
Others take inhaled corticosteroids because they have had their sputum or blood tested, they know their bronchiectasis is an eosinophilic disorder and using an inhaler makes a difference. In a wonderful 2021 patient bronchiectasis conference sponsored by the European Lung Foundation and the European Respiratory Society, Dr. James Chalmers discusses the difference between neutrophilic and eosinophilic inflammation. Dr. Chalmers says that research shows that in 80% of bronchiectasis patients, their condition is neutrophilic and ICS use will not improve their health status. However, in 20% of cases, their inflammation is also eosinophilic and steroids might make a difference. Dr. Colin Swenson and Dr. Wendi Drummond also discuss steroid inhalers in their podcast series NTMTALK.com. Dr. Swenson says that many of us are needlessly on inhalers. Sometimes they are prescribed because of a flare-up. Or, if the person is already on steroids, the dosage is increased. Unfortunately, many remain on high doses even after the flare-up is resolved. My suggestion is that you discuss this issue with your physician and have tests done to determine if ICS use is warranted.Do not take it upon yourself to stop your medication as this could have serious consequences. I have always said, both in my book, “The BE CLEAR Method to Living with Bronchiectasis” and in my social media posts, it is all about EDUCATION. The better we understand our medical condition(s), the better we can ADVOCATE for our care. #bronchiectasis #IBD #RA #osteoporosis #COPD #asthma #celiac #inflammation #lupus Great news!! A fantastic Autogenic Drainage (AD) app that was only available on iPhones is now on Androids! I use this app regularly as part of my daily (often twice a day) clearance and love it.
Sometimes I use it before nebulizing as it helps me to switch gears from working and being on the computer to my self-care. It tells my body to focus on my own care and hopefully let go of mucus. Other times I use the AD app during my airway clearance session– when I’ve used all the tools in my bronchiectasis toolkit including my vest, nebulizing, my Aerobika and postural drainage and that stubborn mucus still doesn’t want to come out. Then there are times I use this breathing technique before and during my session because it only takes 2 minutes–so what not? As I discuss in my recently published book, “The BE CLEAR Method to Living with Bronchiectasis,” it is critical to know airway clearance techniques that do not rely on devices. Because there will be times when you do not have a device with you and start to feel congested. Using “unplugged” methods including breathing techniques and postural drainage will help you feel better. I would suggest you get my book, too! It will give you a map to improving your bronchiectasis self-care and I am always available to answer your questions either by email or social media. Available on Amazon--https://amzn.to/333htls #bronchiectasis #copd #primaryciliarydyskinesia #cysticfibrosis #asthma Chronic lung disease can present intimacy challenges. Concerns about shortness of breath, fatigue, coughing and excess mucus can cause people to shy away from intimate relationships.
To learn how we can address these issues, take a look at this excellent COPD Foundation post by Amanda Atkinson, MSN, RN: https://bit.ly/3y7hkL0 #Intimacy #COPD #oxygenuse #usingoxygen #shortofbreath #breathlessness #emphysema #chronicbronchitis #Bronchiectasis #ChronicCoughing People with bronchiectasis are better educated about diagnostic and treatment options earlier on compared to five years ago, when I was diagnosed. This is thanks to medical organizations, health care institutions and companies like:
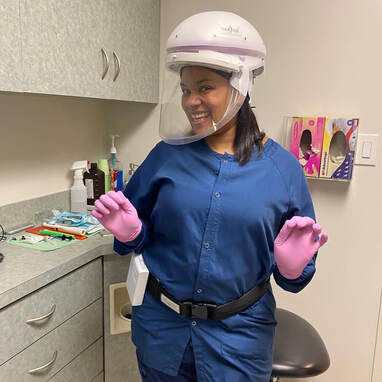
Insmed Bronchiectasis Info and Research NTM Info and Research COPD Foundation’s Bronchiectasis and NTM 360 The European Lung Foundation NYU Langone National Jewish Health Mayo Clinic The result is a well-informed group of people who are being told in webinars they must advocate for the best care for themselves with their health care providers. And THEY DO!! They ask for airway clearance education, medical devices and consultations with specialists. Often, the answer to these requests is “NO, NO, and NO!” I have the opportunity of communicating with dozens of women every week. Our conversations often involve strategies to get providers to listen to their requests seriously. Below are examples from this past week: “I asked for an Aerobika prescription and when I would have my next CT scan. My doctor told me that my BE is mild and I don’t need airway clearance or follow-up scans.” “My BE is progressing and I asked to see a GI doctor to see if I have GERD. My Nurse Practitioner said I don’t have symptoms so I don’t have reflux.” “My doctor told me although I cough non-stop and cannot produce a sputum sample that a bronchoscopy would just irritate me.” “I’m doing airway clearance three times a day, have tons of mucus and asked my doctor for a vibrating vest. She said they are difficult to get and could make my condition worse.” Now, don’t get me wrong. There are superb bronchiectasis centers throughout the US and globally. These doctors are experts in the field of BE and NTM and understand the need for a holistic approach to our disease. But many people do not have the resources to travel to them and must seek care in their communities. With more professional education and the future publication of US bronchiectasis guidelines, this situation will eventually improve. In the meantime, we need to continue to advocate for ourselves and practice daily self-care. #bronchiectasis #selfcare #advocacy For some of us with bronchiectasis, particularly those who also have MAC Lung Disease, going to the dentist can be stressful. Being inverted in a dentist’s chair, having the dental hygienist clean your teeth with an ultrasonic Cavitron spray and then using water from the spit bowl fountain to rinse, can expose us to harmful bacteria as well as cause coughing.
But, if you take some precautions and have good communication with your dental team, it makes all the difference! Consider doing the following:
Good oral hygiene is important for everyone and especially for people with lung disease. There are hundreds of types of oral bacteria –some good, some not so good, and lots we are currently studying because their role is unknown. However, tartar build up and gum disease can be prevented by regular dentist visits. #bronchiectasis #maclungdisease #ntmlungdisease #oralhygiene The “mucociliary escalator” is a term used to describe a built-in mechanism to keep our airways clean. This clearing system is complex, but in the simplest terms, it uses mucus to trap dirt, air pollution particles and pathogens. Then cilia, small hairs that undulate in the moving mucus, sweep the unwanted matter towards our throat where it is expectorated or swallowed.
This cleansing system is ongoing in healthy lungs as they too produce daily mucus to clear the decks. However, in diseased lungs such as those in bronchiectasis (BE), the ciliated areas are damaged and therefore, we make more mucus to compensate. The body does its best to sweep the airways clean, but often it is a herculean task that cannot be automatically accomplished day after day. For this reason, we need to help out our lungs with daily airway clearance. Airway clearance is a broad term describing the effort to help the mucociliary escalator function more effectively. With BE, there are damaged areas in our lungs with little or no cilia allowing mucus to pool. This mucus needs to be removed, otherwise bacteria, viruses and fungi can feed on it and multiply. Whether we use exercise, breathing and coughing techniques, gravity, or medical devices will depend on availability and preferences. What is important is that we do our best to assist our lungs in clearing airways regardless of how often we cough or how much mucus annoys us throughout the day. Working together with our lungs is essential to maintaining overall health and well being. #bronchiectasis #ntmlungdisease #maclungdisease #copd #asthma #lungdisease #lunghealth |
AuthorLinda Cooper Esposito, MPH is a health educator with bronchiectasis. She developed the BE CLEAR Method to Living with Bronchiectasis and writes with compassion and humor about this chronic lung disease. Archives
July 2024
Categories |








 RSS Feed
RSS Feed