|
When it comes to learning airway clearance, NOTHING is better than professional guidance. The problem is respiratory therapists (physios) who specialize in airway clearance techniques, are difficult to find, even where I live in New York City. But, when I found someone, that one session gave me the confidence to begin a daily habit that I will have for the rest of my life.
I’ve since had additional sessions as I continue to learn more and try different approaches. What might work for us today, might not yield the same results in a year or two. And sometimes we just need a tune-up. There are many doctors around the world, both primary care and lung specialists who are not well-versed in airway clearance. But it is my hope that through online education and support groups, we will all understand the importance of keeping our airways clear and will seek out the care we need. It might mean having to raise the subject of services and equipment with your medical team, if they don’t offer those options. Here’s a great analogy to use with your doctor regarding the importance of airway clearance. According to Dr. Pamela McShane, one of the top BE/NTM professionals in the US, we should think of removing mucus from our lungs the way we think of flossing our teeth. We floss even when there doesn’t appear to be anything there, but it breaks up any bacteria biofilm present and is a good habit to have. That is how we can think of trying to remove mucus. We are breaking up biofilm in our lungs. Educate. Advocate. Stay committed. #bronchiectasis #copd #maclungdisease #ntmlungdisease #airwayclearance
0 Comments
I have two diseases–bronchiectasis (BE) and a Mycobacterium Avium Complex (MAC-LD) lung infection. Both were considered rare, but with increased medical professional education and the use of High Resolution CT scans, BE is being diagnosed more frequently than in the past. However, a MAC infection is rare. These bacteria are everywhere in our environment and it is unusual for them to cause disease.
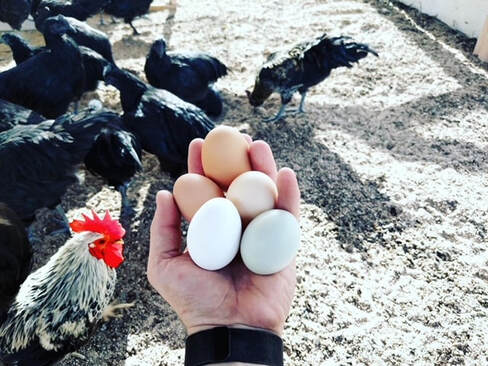
When people are diagnosed with both bronchiectasis and a MAC infection at the same time, which is my situation, doctors frequently say that it is a “chicken or the egg” situation. Did the bronchiectasis damage and inflammation allow the MAC to set up shop in the lungs or did the MAC infection cause the BE? Some answers to this question can be found in a person’s medical and lifestyle history. For example, having pneumonia or bronchitis might have caused the scarring in the lungs, the bronchiectasis. A deeper dive might uncover genetic causes and in some cases, these underlying conditions might be treatable. Although in my case nothing is certain, I probably got the BE from a bad pulmonary infection in my mid-50s that led to inflammation and a welcoming environment for MAC. As I said, MAC is ubiquitous–it is in the soil, water and air. At one point, my husband and I moved out of Manhattan to upstate New York. I had a huge flower garden during the eight years we lived there and spread heaps of mulch and soil. MAC loves mulch and because it is fluffy and easily airborne, it can find its way into the lungs and for some people, cause disease. In my recently published book, “The BE CLEAR Method to Living with Bronchiectasis” https://amzn.to/333htls I mention my double-whammy diseases but focus on bronchiectasis. This was a deliberate choice as there are many people who have BE and will never get MAC or any Nontuberculous Mycobacterial (NTM) infections. At the same time, I feel I should talk about it so that people, if they so choose, can minimize their risk with simple solutions such as wetting soil to prevent dust and wearing a mask while gardening. #bronchiectasis #NTMLungDisease #maclungdisease How does the water we drink that goes into our stomach cause a MAC infection in our lungs?
The answer is two-fold: by inefficient swallowing and gastric reflux. All of us micro-aspirate liquid into our lungs throughout the day. This might be from liquid “going down the wrong pipe” as can happen with swallowing issues, coughing, or “just because.” Although a certain number of aspirations is considered normal and not a concern for those with healthy immune systems and lungs, this may not be the case for people with impaired airways. Gastroesophogeal Reflux is another way bacteria can enter the lungs. Both acid and non-acid gastric refluxate can come up from the stomach and enter the lungs. This liquid can contain bacteria that have not been killed off by our stomach acid and possibly cause infection. One way to help prevent reflux is to take GERD precautions. These precautions might include:
In addition to reducing swallowing issues and GERD, we can also reduce the MAC in our drinking water. Boiling water for 10 minutes or drinking spring water will greatly reduce this exposure and is something I do. If you choose to drink spring water, do not drink from a water cooler as a MAC biofilm might be lining the inside of the machine. The same is true for refrigerator filtered water and ice and Brita-like charcoal pitchers. Not everyone with bronchiectasis will get a MAC infection. However, there is about a 10-20% chance you will and the precautions I have laid out can reduce that probability. Some BE and MAC specialists tell their patients to just live their lives and to not try to control bacteria that is everywhere in our environment. Others suggest taking preventive measures. So it is best to have this conversation with your doctors and see what they recommend. Remember, we have a life-long condition so you can always make changes gradually over time. #bronchiectasis #maclungdisease #ntmlungdisease #GERD The “B” in my book, “The BE CLEAR Method to Living with Bronchiectasis,” stands for “Breathing.” To breathe our best we need to create space in our body by lengthening our spine. In other words, by improving our posture.
During a 2021 patient bronchiectasis conference, Dr. Jonathan Whiteson, Medical Director of the NYU Langone Cardiopulmonary Rehabilitation department, repeatedly mentioned the connection between good posture and lung health. Improving posture begins with believing it is critical to your well-being. It means that you too believe that sitting, standing and walking more upright will lead to better breathing and many other benefits including: * More confidence * Less coughing * Less feeling short of breath * Better digestion including less gastric reflux * More stability while walking * Fewer joint issues Like any new habit, improving your posture will require daily practice. For example, write the phrase “lengthen your spine” or “sit with better posture” on a slip of paper and put it on the table when you eat, or when you are at your desk or watching TV. Observe what might be getting in your way of sitting, standing and walking more upright. See what you can do to address these challenges. In my book, “The BE CLEAR Method,” I demonstrate 10 exercises to improve your strength and alignment. Some people with BE have spinal issues such as scoliosis and kyphosis, but understanding the importance of posture and making small changes to better align the spine, will make a difference over time. As your body begins to elongate you will feel the difference. Your breath will have more room to naturally flow more evenly and deeply. #bronchiectasis #copd #breathing #posture |
AuthorLinda Cooper Esposito, MPH is a health educator with bronchiectasis. She developed the BE CLEAR Method to Living with Bronchiectasis and writes with compassion and humor about this chronic lung disease. Archives
April 2024
Categories |




 RSS Feed
RSS Feed